The impact of stressful events on the Brain-Gut axis
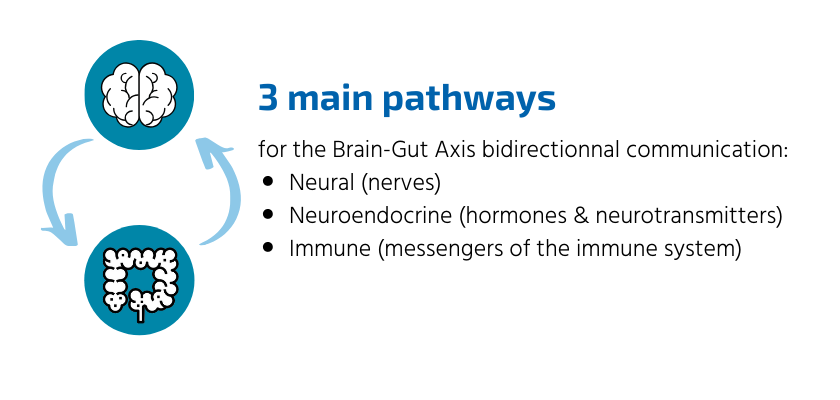
Over time, advances in research have revealed additional evidence that bidirectional communication takes place between these structures, and that it intensifies in times of stress.
Common physical reactions when experiencing an acute stressful event
However, when the stress response is sustained, it can have a negative effect on parts of the body, including the digestive system.
When experiencing a stressful event, the area of the brain that controls emotions, the amygdala, sends a distress signal to the hypothalamus, the brain’s command center. The hypothalamus then sends out an alert through the nervous system, which responds by releasing a flood of stress hormones, including adrenaline and cortisol. In turn, these hormones prepare the body for emergency action, known as the fight-or-flight response. When activated, digestion slows as the body uses its energy resources on the threat at hand, and in turn, increases gut sensitivity. Common physical symptoms of acute stress include a pounding heart, tightening of muscles, a rise in blood pressure, and rapid breathing. These physical changes increase strength and stamina, improve reaction time, and enhance focus, preparing to either fight or escape in response to the stressful situation.
Chronic stress takes a toll on the body
When the body is repeatedly exposed to stress, it can initiate a vicious cycle of inflammation. Inflammation and the action of the pathogens can lead to increased barrier permeability (also known as leaky gut). This disruption will allow bacterial translocation and inflammation signals through the vagus nerve, from the gut to the brain. The brain interprets this inflammation signal as a new stressor. These stressors combine with potential external stressors will eventually lead to psychological, physiological, and behavioral symptoms. The findings of Maes et al. published in 2012, suggest that “translocated” gut commensal bacteria activate immune cells to elicit antibodies (IgA and IgM) responses; this phenomenon may play a role in the pathophysiology of (chronic) depression through the progressive amplification of immune pathways.